百草枯(paraquat,PQ)是一种高效接触型除草剂,由于其进入泥土后迅速失活且无残留,具有环保高效的优点,因此被全世界广泛用于农业生产。PQ对人畜具有强毒性,人类经口摄入20%PQ水溶液达15~20 mL即可致死[1],急性PQ中毒往往可损伤患者肺、肾及肝等多个器官,病死率高达60%~80%[2];肺组织为PQ中毒损伤的靶器官,早期严重的肺水肿以及后期出现的不可逆肺纤维化是PQ中毒的主要病理变化[3-6]。目前PQ中毒的治疗方法主要有洗胃催吐、利尿导泻、血液净化、抗氧化、肺移植等[7-8],然而,这些方法的有效性尚不明确,因此PQ中毒患者病死率极高。PQ中毒的致病机制主要与氧化应激和炎症损伤有关[9-11],其中炎症反应为当前研究热点,值得关注的是,近年来已有不少研究发现白细胞、中性粒细胞、中性粒细胞与淋巴细胞比值(neutrophil to lymphocyte ratio,NLR)等炎症指标与PQ中毒患者预后相关[12-15],这进一步提示PQ中毒与炎症反应有密切联系。
单核细胞与淋巴细胞比值(monocytes to lymphocyte ratio,MLR)作为一个新型的炎症指标[16],可直接从血常规中计算获得,具有成本低廉、检测方便、快速等优点,已被用于多种与炎症损伤相关疾病的评估,如肿瘤、缺血性脑卒中、冠心病等[17-19],然而目前尚无研究探讨MLR与急性PQ中毒患者全因死亡的关系。因此,本文旨在研究MLR与急性PQ中毒患者预后之间的关系,以及评估MLR对急性PQ中毒患者死亡风险的预测价值。
1 资料与方法本次研究对象匿名,不涉及对患者的任何干预措施,患者入院均已签署知情同意书。
1.1 一般资料回顾性选取2013年12月年至2018年10月收治于南昌大学第一附属医院的急性PQ中毒患者117例,研究对象均有明确口服中毒史、临床症状及符合PQ中毒诊断标准。随访至截止时间。主要终点事件为全因死亡。纳入标准:①中毒至入院时间≤24 h;②年龄≥14岁。排除标准:①服毒时间不详;②混合其他农药或药物中毒;③怀孕期服毒;④近期合并其他感染;⑤慢性阻塞性肺疾病(慢性支气管炎、肺气肿等);⑥血液病;⑦长期服用免疫抑制剂(糖皮质激素);⑧肿瘤;⑨合并心、脑、肾、肝等重要脏器基础疾病;⑩资料缺失或失访。具体流程见图 1。
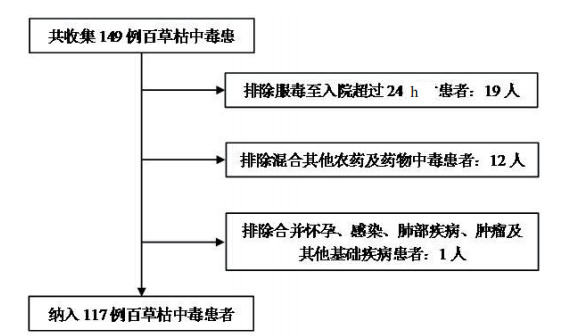
|
| 图 1 流程图 Fig 1 Flow chart of the included patients |
|
|
所有患者均按PQ中毒原则接受治疗:①清除毒物(洗胃导泻、补液利尿、血液净化等);②抗氧化剂治疗;③免疫抑制剂治疗;④抗肺纤维化及器官支持。
1.3 资料收集收集患者资料(包括年龄、性别、体温、心率、收缩压、呼吸频率、烟酒史、高血压、糖尿病、服毒量和急性生理和慢性健康评估Ⅱ(acute physiology and chronic health evaluation-Ⅱ,APACHE Ⅱ)评分,以及入院首次抽血化验指标:白细胞、血小板、单核细胞、淋巴细胞、血红蛋白、血白蛋白、丙氨酸转氨酶、血总胆红素、血肌酐、肌酸激酶、肺泡氧分压、血气pH及血钾值),为避免误差,以上资料由两名临床医生共同采集并进行核对,所有资料均从南昌大学第一附属医院电子病历系统获得。MLR为单核细胞与淋巴细胞计数的比值。生存时间通过病历记录及电话随访确定。
1.4 统计学方法采用SPSS 21.0软件进行统计学分析。近似正态分布计量资料采用均数标准差(Mean±SD)描述,非正态分布的计量资料采用中位数和四分位间距描述;计数资料采用总数和百分比描述;计量资料的组间比较如符合正态分布采用ANOVA单因素分析,如不符合正态分布采用Kruskal-Wallis检验,计数资料的组间比较采用卡方检验;采用Kaplan-Meier曲线分析患者累积生存率;Cox多因素回归模型分析急性PQ中毒患者的独立危险因素,结果以风险比(hazard ratio,HR)±95%置信区间(confidence interval,CI)表示;采用受试者工作特性(receiver-operating characteristic,ROC)曲线评估MLR对PQ中毒患者全因死亡的预测价值。以P < 0.05为差异有统计学意义。
2 结果 2.1 患者一般情况本研究共纳入117例患者,其中男49例,女68例,年龄(36.91±16.00)岁。随访至截至日期,病死率为59.8%(70/117)。表 1列出了基于MLR值平均分为四组(Quartile 1: MLR≤0.22,Quartile 2: MLR 0.22~0.37,Quartile 3: MLR 0.37~0.71,Quartile 4: MLR > 0.71)的患者人口学特征与临床数据的基线资料。由结果示,与Quartile 1相比,Quartile 4患者的白细胞、单核细胞、血MLR值、血气pH、血肌酐值较高,而淋巴细胞数则较低;各组患者年龄、性别及入院时一般情况均差异无统计学意义(P > 0.05)。
| 指标 | Total (n=117) | Quartile 1 (n=29) | Quartile 2 (n=30) | Quartile 3 (n=29) | Quartile 4 (n=29) | P值 |
| 年龄(岁) | 36.91±16.00 | 36.48±14.39 | 39.33±14.24 | 30.48±14.97 | 41.24±18.73 | 0.322 |
| 性别(男/女) | 49/68 | 12/17 | 11/19 | 13/16 | 13/16 | 0.077 |
| 体温(℃) | 36.50±0.38 | 36.47±0.32 | 36.54±0.40 | 36.52±0.34 | 36.47±0.45 | 0.080 |
| 心率(次/min) | 83.10±15.56 | 80.97±13.07 | 81.07±12.23 | 88.93±14.85 | 81.52±20.24 | 0.610 |
| 收缩压(mmHg) | 124.10±18.61 | 124.66±18.12 | 121.27±14.61 | 120.90±16.55 | 129.66±23.68 | 0.845 |
| 呼吸频率(次/min) | 19.96±5.38 | 19.59±4.02 | 19.07±3.89 | 20.90±7.71 | 20.31±5.17 | 0.350 |
| 吸烟(是/否) | 15/102 | 5/24 | 6/24 | 2/27 | 2/27 | 0.282 |
| 高血压(是/否) | 11/106 | 4/25 | 2/28 | 3/26 | 2/27 | 0.769 |
| 糖尿病(是/否) | 1/116 | 1/28 | 0/30 | 0/29 | 0/29 | 0.421 |
| 服用PQ剂量(mL) | 35(15, 97.5) | 40(10, 60) | 20(10, 50) | 25(15, 60) | 70(30, 100) | 0.009 |
| 血气分析pH | 7.41(7.39, 7.44) | 7.41(7.39, 7.44) | 7.44(7.41, 7.46) | 7.41(7.39, 7.44) | 7.39(7.32, 7.42) | 0.001 |
| APACHE-Ⅱ评分 | 4(2, 9.75) | 5(2.75, 11.25) | 3(2, 5) | 3(1, 9) | 9(4, 16) | 0.007 |
| 血白细胞(×109/L) | 13.84(9.45, 19.36) | 10.01(8.28, 18.72) | 10.02(7.21, 12.13) | 14.84(10.47, 19.33) | 19.67(15.86, 31.41) | < 0.001 |
| 血红蛋白(g/L) | 139.85±18.37 | 135.10±15.84 | 136.70±19.68 | 142.38±19.11 | 145.31±17.58 | 0.114 |
| 单核细胞(×109/L) | 0.42 (0.23, 0.65) | 0.15 (0.05, 0.23) | 0.36 (0.24, 0.42) | 0.48 (0.37, 0.63) | 0.84 (0.61, 1.43) | < 0.001 |
| 淋巴细胞(×109/L) | 0.97 (0.71, 1.35) | 1.07 (0.84, 2.30) | 1.20 (0.77, 1.44) | 0.93 (0.69, 1.17) | 0.79 (0.60, 1.20) | 0.012 |
| 血清MLR | 0.37 (0.22, 0.71) | 0.17 (0.04, 0.19) | 0.28 (0.25, 0.33) | 0.54 (0.46, 0.62) | 1.02 (0.91, 1.32) | < 0.001 |
| 谷丙转氨酶(U/L) | 19 (16, 33.5) | 17 (12, 52) | 16.5 (12, 25) | 19 (11, 31) | 26 (19, 56) | 0.078 |
| 血总胆红素(mmol/L) | 13.3 (9.7, 18.75) | 14.6 (9.85, 22.8) | 12.75 (9.98, 16.12) | 13.5 (9.55, 20.0) | 13.8 (10.85, 19.4) | 0.239 |
| 血白蛋白(g/L) | 42.9 (39.55, 45.95) | 42.5 (40.3, 44.5) | 42.4 (39.25, 44.9) | 43.6 (38.6, 48.2) | 44.9 (41.45, 46.9) | 0.226 |
| 血肌酐(mmol/L) | 102.8 (61.1, 217.7) | 97.7 (54.55, 250.3) | 62.7 (54.18, 90.23) | 118 (77.1, 223.05) | 174.7 (94.85, 269.5) | 0.001 |
| 肌酸激酶(U/L) | 143 (90.5, 274.5) | 158 (104.5, 300.5) | 100 (74.75, 145.75) | 146 (89, 284.5) | 244 (122, 518.5) | 0.001 |
| 血钾(mmol/L) | 3.80±0.61 | 3.87±0.66 | 3.76±0.35 | 3.86±0.66 | 3.71±0.70 | 0.725 |
| 注:(1 mmHg=0.133 kPa,1 cmH2O=0.098 kPa) | ||||||
ROC曲线结果如图 2所示,确定MLR预测全因病死率的最佳截断值为0.61,曲线下面积(area under the curve,AUC)为0.684 (95%CI: 0.591~0.767,P=0.0002),敏感性为47.14%,特异性为91.49%。
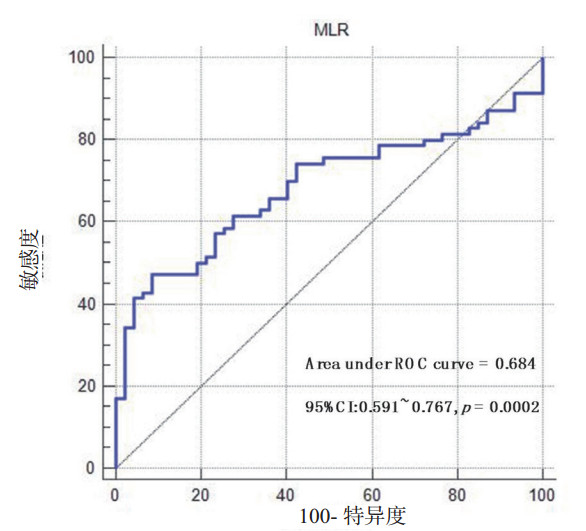
|
| MLR为单核细胞与淋巴细胞比值 图 2 MLR预测急性百枯中毒患者全因死率ROC曲线 Fig 2 The ROC curve of MLR predicting all-cause mortality in patients with acnte paraqnat poisoning |
|
|
Kaplan-Meier生存分析(图 3)显示Quartile 4的累积生存率较Quartile 1、Quartile 2和Quartile 3低(log-rank=33.376,P < 0.01)。根据MLR最佳截断值0.61将研究人群分为两组做相同分析(图 4),与MLR < 0.61的患者相比,MLR≥0.61患者的终点事件发生率明显更高(log-rank=26.451,P < 0.01)。纳入与PQ中毒患者全因死亡相关的风险因素后进行多因素Cox回归分析(表 2),结果表明,当校正年龄、性别、糖尿病、高血压、吸烟、呼吸频率、血红蛋白、血白蛋白及血肌酐值后,Quartile 4比Quartile 1的死亡风险更高(HR=2.773,95%CI: 1.250~6.154, P=0.012)。
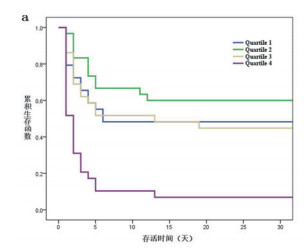
|
| 图 3 4组百草枯中毒患者Kaplan-Meier生存曲线 Fig 3 The Kaplan-Meier curve of patients with paraquat poisoning in Quartiles 1, 2, 3 and 4 |
|
|
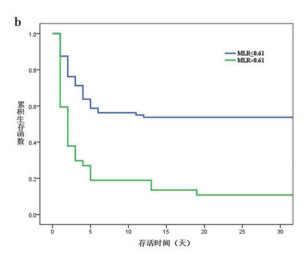
|
| 图 4 2组百草枯中毒患者Kaplan-Meier生存曲线 Fig 4 The Kaplan-Meier curve of patients with paraquat poisoning with MLR ≤0.61 and > 0.61 |
|
|
| MLR | Quartile 1 (≤0.22) | Quartile 2 (0.22~0.37) | Quartile 3 (0.37~0.71) | Quartile 4 (>0.71) |
| 未校正模型 | ||||
| HR (95%CI) | 参考 | 0.664 (0.311~1.419) | 1.055 (0.522~2.135) | 3.095(1.625~5.892) |
| P值 | - | 0.291 | 0.881 | 0.001 |
| 校正模型 | ||||
| 模型A | ||||
| HR (95%CI) | 参考 | 0.626(0.292~1.345) | 1.174(0.572~2.413) | 3.037(1.587~5.811) |
| P值 | - | 0.230 | 0.662 | 0.001 |
| 模型B | ||||
| HR (95%CI) | 参考 | 0.683(0.312~1.496) | 1.223(0.582~2.571) | 3.292(1.665~6.510) |
| P值 | - | 0.341 | 0.596 | 0.001 |
| 模型C | ||||
| HR (95%CI) | 参考 | 0.707(0.310~1.162) | 0.893(0.409~1.953) | 2.773(1.250~6.154) |
| P值 | - | 0.410 | 0.778 | 0.012 |
| 模型A:校正年龄、性别;模型B:校正模型A及糖尿病、高血压、吸烟;模型C:校正模型B及呼吸频率、血红蛋白、血白蛋白、血肌酐值 | ||||
本研究探讨了入院时血MLR水平与急性PQ中毒患者病死率之间的关系,在本研究中,发现高MLR组患者的累计生存率明显低于其他较低MLR组,同时,基于最佳截断MLR值0.61分组的分析也发现了相同的趋势。此外,还发现在调整了相关危险因素后,MLR是急性PQ中毒患者全因病死率的一个重要的、独立的预测因子。
农药中毒是我国的一个重要公共健康问题,其中,急性PQ中毒由于进展快、预后差、无特效治疗措施,近年来引起了人们广泛关注[20],据报道,2002-2011年间我国PQ中毒发生率持续上升[21],尽管2012年起国内外已禁止生产和销售PQ,PQ中毒事件增长速度有所减缓,但我国为农业大国,PQ存贮量巨大,近年PQ中毒发病率仍呈现上升趋势。因此寻找一个可靠的可用于预测PQ中毒患者死亡风险的指标至关重要。
血浆PQ浓度是被认为是预测PQ中毒病死率准确、可靠的指标[22-24],然而,该指标检测费用昂贵且许多医院尚不具备相关检测设备,因此,该指标的临床适用性不高。与血浆PQ浓度相比,MLR是一个计算简便、廉价的指标。近年来,MLR已被认为是内皮功能障碍和炎症的代用指标,具有一定的预后和预测价值[16];MLR作为一种新型的炎症预测因子,许多研究证明MLR与多种疾病的死亡预后相关[25-28],Yuan等[29]研究表明MLR越高,非小细胞肺癌患者的死亡风险越高,而Choi, 等[30]在研究中也发现MLR值可独立预测胆囊癌化疗患者的生存率。
单核细胞是白细胞的一种亚型,具有分化成巨噬细胞及树突状细胞的潜力,当前许多研究认为,单核细胞计数升高与各种疾病的不良预后有密切关系[31-33]。作为机体免疫的重要成员,单核细胞在PQ中毒机制中的作用逐渐引起人们关注,有研究表明,PQ可诱导骨髓间充质干细胞快速表达单核细胞趋化蛋白-1,使血液中单核细胞迅速增多[34-35];活化的单核细胞聚集在肺内,促进趋化因子和促炎因子(如TNF-α和IL-8)的产生,激活炎症反应,其次,来源于单核细胞的肺泡巨噬细胞可启动免疫反应并产生活性氧,导致细胞NADPH耗竭和细胞膜脂质过氧化,同时,肺泡巨噬细胞产生的转化生长因子,可促进成纤维细胞中促纤维化基因的表达,导致组织纤维化。淋巴细胞是机体主要的免疫细胞,参与炎症反应的调控,淋巴细胞减少常见于心肌缺血、生理应激、皮质醇和儿茶酚胺水平升高,以及严重炎症反应导致淋巴细胞凋亡的患者。PQ中毒引起淋巴细胞绝对值下降的具体机制尚未明确,可能与PQ引起氧化应激使体内氧自由基(ROS)及皮质醇激素产生增多,进而诱导淋巴细胞凋亡有关。
目前已有研究表明,高单核细胞和低淋巴细胞均可作为预测PQ中毒预后的独立风险指标,然而,相比于单核细胞或淋巴细胞绝对值,MLR可能是更好的预测指标,理由如下:首先,MLR相对于单个单核细胞或淋巴细胞计数更稳定,更不容易被不同的生理病理条件改变;其次,使用比值方式可消除系统误差,减少误差干扰,提高统计效能;最后,MLR结合了单核细胞与淋巴细胞两个指标的意义,增强指标的说服力与可靠性;因此采用MLR作为预测急性PQ中毒预后的指标会更加理想。
利益冲突 所有作者均声明不存在利益冲突。
| [1] | Wunnapuk K, Mohammed F, Gawarammana I, et al. Prediction of paraquat exposure and toxicity in clinically ill poisoned patients: a model based approach[J]. Br J Clin Pharmacol, 2014, 78(4): 855-866. DOI:10.1111/bcp.12389 |
| [2] | Weng CH, Hu CC, Lin JL, et al. Predictors of acute respiratory distress syndrome in patients with paraquat intoxication[J]. PLoS One, 2013, 8(12): e82695. DOI:10.1371/journal.pone.0082695 |
| [3] | Schapochnik A, da Silva MR, Leal MP, et al. Vitamin D treatment abrogates the inflammatory response in paraquat-induced lung fibrosis[J]. Toxicol Appl Pharmacol, 2018, 355: 60-67. DOI:10.1016/j.taap.2018.06.020 |
| [4] | Harchegani AL, Hemmati AA, Nili-Ahmadabadi A, et al. Cromolyn sodium attenuates paraquat-induced lung injury by modulation of proinflammatory cytokines[J]. Drug Res (Stuttg), 2017, 67(5): 283-288. DOI:10.1055/s-0042-123711 |
| [5] | Sun B, Chen YG. Advances in the mechanism of paraquat-induced pulmonary injury[J]. Eur Rev Med Pharmacol Sci, 2016, 20(8): 1597-1602. |
| [6] | 符红娜, 聂时南. 百草枯致肺纤维化的上皮-间质转化的机制研究进展[J]. 中华急诊医学杂志, 2019, 28: 803-805. DOI:10.3760/cma.j.issn.1671-0282.2019.06.033 |
| [7] | Sun BS, He YZ. Paraquat poisoning mechanism and its clinical treatment progress[J]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue, 2017, 29(11): 1043-1046. DOI:10.3760/cma.j.issn.2095-4352.2017.11.018 |
| [8] | Wu WP, Lai MN, Lin CH, et al. Addition of immunosuppressive treatment to hemoperfusion is associated with improved survival after paraquat poisoning: a nationwide study[J]. PLoS One, 2014, 9(1): e87568. DOI:10.1371/journal.pone.0087568 |
| [9] | Ahmed MAE, El Morsy EM, Ahmed AAE. Protective effects of febuxostat against paraquat-induced lung toxicity in rats: Impact on RAGE/PI3K/Akt pathway and downstream inflammatory cascades[J]. Life Sci, 2019, 221: 56-64. DOI:10.1016/j.lfs.2019.02.007 |
| [10] | Yang W, Liu W, Yu W, et al. Angptl2 deficiency attenuates paraquat (PQ)-induced lung injury in mice by altering inflammation, oxidative stress and fibrosis through NF-κB pathway[J]. Biochem Biophys Res Commun, 2018, 503(1): 94-101. DOI:10.1016/j.bbrc.2018.05.186 |
| [11] | Liu MW, Su MX, Zhang W, et al. Protective effect of Xuebijing injection on paraquat-induced pulmonary injury via down-regulating the expression of p38 MAPK in rats[J]. BMC Complement Altern Med, 2014, 14: 498. DOI:10.1186/1472-6882-14-498 |
| [12] | Chen HL, Hu LF, Li HZ, et al. An effective machine learning approach for prognosis of paraquat poisoning patients using blood routine indexes[J]. Basic Clin Pharmacol Toxicol, 2017, 120(1): 86-96. DOI:10.1111/bcpt.12638 |
| [13] | Feng SY, Gao J, Li Y. A retrospective analysis of leucocyte count as a strong predictor of survival for patients with acute paraquat poisoning[J]. PLoS One, 2018, 13(7): e0201200. DOI:10.1371/journal.pone.0201200 |
| [14] | Liang H, Gao Y, Liu Y, et al. Predictive value of neutrophil-to-lymphocyte ratio in 30-day mortality of patients with acute paraquat poisoning[J]. Chin J Ind Hyg Occup Dis, 2018, 36(12): 911-914. DOI:10.3760/cma.j.issn.1001-9391.2018.12.007 |
| [15] | Zhou DC, Zhang H, Luo ZM, et al. Prognostic value of hematological parameters in patients with paraquat poisoning[J]. Sci Rep, 2016, 6: 36235. DOI:10.1038/srep36235 |
| [16] | Balta S, Demırer Z, Aparci M, et al. The lymphocyte-monocyte ratio in clinical practice[J]. J Clin Pathol, 2016, 69(1): 88-89. DOI:10.1136/jclinpath-2015-203233 |
| [17] | Stotz M, Szkandera J, Stojakovic T, et al. The lymphocyte to monocyte ratio in peripheral blood represents a novel prognostic marker in patients with pancreatic cancer[J]. Clin Chem Lab Med, 2015, 53(3): 499-506. DOI:10.1515/cclm-2014-0447 |
| [18] | Ren H, Liu X, Wang L, et al. Lymphocyte-to-monocyte ratio: a novel predictor of the prognosis of acute ischemic stroke[J]. J Stroke Cerebrovasc Dis, 2017, 26(11): 2595-2602. DOI:10.1016/j.jstrokecerebrovasdis.2017.06.019 |
| [19] | Murat SN, Yarlioglues M, Celik IE, et al. The relationship between lymphocyte-to-monocyte ratio and bare-metal stent in-stent restenosis in patients with stable coronary artery disease[J]. Clin Appl Thromb Hemost, 2017, 23(3): 235-240. DOI:10.1177/1076029615627340 |
| [20] | 卢中秋. 精益求精, 进一步提高我国急诊中毒临床诊治水平[J]. 中华急诊医学杂志, 2019, 28: 275-278. DOI:10.3760/cma.j.issn.1671-0282.2019.03.001 |
| [21] | Yin Y, Guo X, Zhang SL, et al. Analysis of paraquat intoxication epidemic (2002-2011) within China[J]. Biomed Environ Sci, 2013, 26(6): 509-512. DOI:10.3967/0895-3988.2013.06.014 |
| [22] | Senarathna L, Eddleston M, Wilks MF, et al. Prediction of outcome after paraquat poisoning by measurement of the plasma paraquat concentration[J]. QJM, 2009, 102(4): 251-259. DOI:10.1093/qjmed/hcp006 |
| [23] | Hong SY, Lee JS, Sun IO, et al. Prediction of patient survival in cases of acute paraquat poisoning[J]. PLoS One, 2014, 9(11): e111674. DOI:10.1371/journal.pone.0111674 |
| [24] | Du Y, Mou Y. Predictive value of 3 methods in severity evaluation and prognosis of acute paraquat poisoning[J]. J Central South Univ Med Sci, 2013, 38(7): 737-742. DOI:10.3969/j.issn.1672-7347.2013.07.014 |
| [25] | Wang L, Long W, Li PF, et al. An elevated peripheral blood monocyte-to-lymphocyte ratio predicts poor prognosis in patients with primary pulmonary lymphoepithelioma-like carcinoma[J]. PLoS One, 2015, 10(5): e0126269. DOI:10.1371/journal.pone.0126269 |
| [26] | Shi LH, Qin XQ, Wang HJ, et al. Elevated neutrophil-to-lymphocyte ratio and monocyte-to-lymphocyte ratio and decreased platelet-to-lymphocyte ratio are associated with poor prognosis in multiple myeloma[J]. Oncotarget, 2017, 8(12): 18792-18801. DOI:10.18632/oncotarget.13320 |
| [27] | Xiang FF, Chen RY, Cao XS, et al. Monocyte/lymphocyte ratio as a better predictor of cardiovascular and all-cause mortality in hemodialysis patients: a prospective cohort study[J]. Hemodial Int, 2018, 22(1): 82-92. DOI:10.1111/hdi.12549 |
| [28] | Fan ZY, Li Y, Ji HH, et al. Prognostic utility of the combination of monocyte-to-lymphocyte ratio and neutrophil-to-lymphocyte ratio in patients with NSTEMI after primary percutaneous coronary intervention: a retrospective cohort study[J]. BMJ Open, 2018, 8(10): e023459. DOI:10.1136/bmjopen-2018-023459 |
| [29] | Yuan C, Li N, Mao XY, et al. Elevated pretreatment neutrophil/white blood cell ratio and monocyte/lymphocyte ratio predict poor survival in patients with curatively resected non-small cell lung cancer: Results from a large cohort[J]. Thorac Cancer, 2017, 8(4): 350-358. DOI:10.1111/1759-7714.12454 |
| [30] | Choi YH, Lee JW, Lee SH, et al. A high monocyte-to-lymphocyte ratio predicts poor prognosis in patients with advanced gallbladder cancer receiving chemotherapy[J]. Cancer Epidemiol Biomarkers Prev, 2019, 28(6): 1045-1051. DOI:10.1158/1055-9965.EPI-18-1066 |
| [31] | Balın Ö, Tartar AS, Akbulut A. The predictive role of haematological parameters in the diagnosis of osteoarticular brucellosis[J]. Afr Health Sci, 2018, 18(4): 988-994. DOI:10.4314/ahs.v18i4.19 |
| [32] | Feng F, Zheng GZ, Wang Q, et al. Low lymphocyte count and high monocyte count predicts poor prognosis of gastric cancer[J]. BMC Gastroenterol, 2018, 18(1): 148. DOI:10.1186/s12876-018-0877-9 |
| [33] | Moon JM, Chun BJ, Cho YS, et al. Diagnostic value of parameters related to white blood cell counts for troponin I elevation in CO poisoning[J]. Cardiovasc Toxicol, 2019, 19(4): 334-343. DOI:10.1007/s12012-018-09501-w |
| [34] | Shi C, Jia T, Mendez-Ferrer S, et al. Bone marrow mesenchymal stem and progenitor cells induce monocyte emigration in response to circulating toll-like receptor ligands[J]. Immunity, 2011, 34(4): 590-601. DOI:10.1016/j.immuni.2011.02.016 |
| [35] | Amirshahrokhi K, Khalili AR. Carvedilol attenuates paraquat-induced lung injury by inhibition of proinflammatory cytokines, chemokine MCP-1, NF-κB activation and oxidative stress mediators[J]. Cytokine, 2016, 88: 144-153. DOI:10.1016/j.cyto.2016.09.004 |
 2021, Vol. 30
2021, Vol. 30




