传统理论认为,急性ST段抬高型心肌梗死(ST-segment elevation myocardial infarction, STEMI)多为单支血管闭塞性病变,冠脉内为富含纤维蛋白的红色血栓,治疗原则是在强化抗栓、抗缺血的基础上,尽早、完全、持续开通梗死相关动脉,可行溶栓或急诊介入治疗[1-2];而非ST段抬高型心肌梗死(non-ST-segment elevation myocardial infarction, NSTEMI)为多支血管非闭塞性病变,冠脉内为富含血小板的白色血栓,治疗原则是强化抗栓、抗缺血治疗,必要时可行急诊介入治疗,而溶栓是绝对禁忌证[3]。而研究发现,NSTEMI患者的冠脉造影和冠脉内血栓类型与STEMI患者存在交叉情况。Grenne等[4]报道,3l%的NSTEMI患者的梗死相关血管为闭塞血管;一项荟萃分析报道[5],合并有闭塞性罪犯血管的NSTEMI患者占34%,且闭塞性罪犯血管多为左回旋支。Ino等[6]应用光学相干断层成像(optical coherence tomography, OCT)对49例非ST段抬高型急性冠脉综合征(non-ST-segment elevation acute coronary syndrome, NSTEACS)患者的病变血管进行观察,结果示13例患者冠脉内为红色血栓,19例患者冠脉内为白色血栓。
课题组前期研究发现,急性非ST段抬高型心肌梗死患者中存在一类患者,其心电图表现为ST段较基线无明显偏移,其临床特征有别于ST段压低的急性心肌梗死(acute myocardial infarction, AMI)患者。因此,本文在前期的工作基础上[7-8],将AMI根据心电图ST段位移特点分为三种类型:ST段抬高型、ST段无偏移型和ST段压低型,研究AMI心电图ST段不同改变与冠脉造影和血栓类型的相关关系。
1 资料与方法 1.1 一般资料连续纳入2016年9月至2018年8月因AMI就诊于河南省人民医院,于发病24 h内行急诊冠脉介入治疗的患者。AMI的诊断采取2018年ESC公布的第4版全球心肌梗死的标准定义[9]。排除严重的左主干病变及冠状动脉严重迂曲、钙化或成角病变。
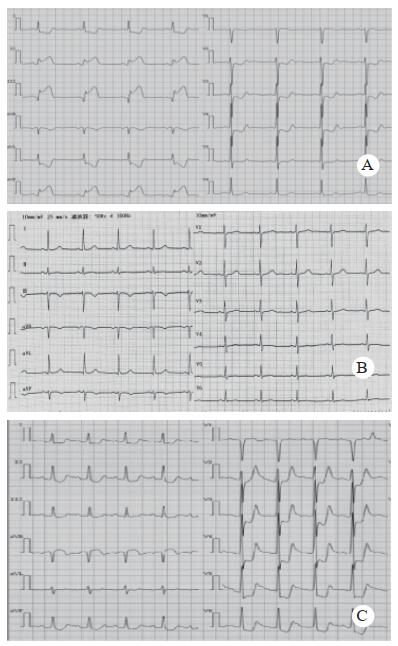
1.2 分组根据12导联心电图ST段改变将患者分为ST段抬高组、ST段无偏移组和ST段压低组,见图 1。ST段改变的诊断标准参考2009年心电图标准化及解析指南[10]。其中,ST段抬高:连续2个以上导联ST段抬高(胸前导联≥2 mm,肢体导联≥1 mm);ST段压低型:连续2个以上导联ST段呈水平型或下斜型压低(胸前导联≥2 mm,肢体导联≥1 mm);ST段无偏移:无明显ST段移位。
|
| A:ST段抬高型; B:ST段无偏移型; C:ST段压低型 图 1 急性心肌梗死心电图ST段表现 Fig 1 changes of ST segment in acute myocardial infarction |
|
|
由本院心脏导管室2名固定的有经验的心脏介入科医师对患者行急诊冠脉造影。记录梗死相关动脉(infarction related artery, IRA)、梗死部位、是否闭塞病变、有无侧支循环以及病变血管支数等,如二者的造影报告存在争议,则回顾造影光盘后商讨确认。
1.3.2 光学相干断层成像检查本研究采用频域OCT成像导管进行图像采集(ILUMIEN OPTIS OCT血管内成像系统,雅培医疗,美国)。当TIMI血流≤2级时先进行血栓抽吸。将指引导管放于左或右冠状动脉口,将导丝送至入梗死相关血管远端。将OCT阻断球囊导管沿导丝送入病变部位的远端。沿OCT阻断球囊导管将OCT成像导丝送至病变部位的远端。撤出OCT阻断球囊导管,使球囊标记点撤至血管病变段的近端。设定流速及压力,对血管腔进行冲洗的同时充盈OCT阻断球囊堵塞血管。当确认OCT的同轴性比较好且图像清晰时,开始回撤成像导丝并进行OCT的扫描成像。成像结束后,迅速负压抽回阻断球囊导管,停止对其冲洗。将OCT的球囊导管和成像导丝缓慢回撤至指引导管内。
1.3.3 OCT影像资料分析所有的OCT图像由2位经过培训的专业分析人员应用OCT自带软件进行分析。OCT鉴别冠脉内血栓类型的标准:红色血栓:呈高背反射,半透光伴阴影;白色血栓:呈低背反射、信号均一且无阴影。
1.4 临床资料收集收集患者的临床基线资料,包括年龄、性别、吸烟史、饮酒史、高血压病史、糖尿病病史、血脂异常、脑卒中病史、冠心病家族史、既往心肌梗死及心绞痛病史、既往PCI史、抗血小板药物及他汀类药物服用史及入院后左室射血分数(left ventricular ejection fraction, LVEF)。
1.5 统计学方法采用SPSS22.0统计软件处理数据。采用S-W检验对计量资料的正态性进行检验,当计量资料服从正态分布时,以均数±标准差(Mean±SD)表示,组间比较采用单因素方差分析,进一步两两比较采用Bonferroni-t法;不符合正态分布的计量资料用中位数(四分位数)进行统计描述,采用Kruskal-Wallis秩和检验进行组间差异性比较。计数资料通过频数(百分比)表示,多组样本间率的比较采用卡方检验,当≥2个格子期望值小于5或者≥1个格子期望值小于1时,采用Fisher确切概率法。以P < 0.05为差异有统计学意义。
2 结果 2.1 3组患者临床资料比较3组患者在性别(P<0.001)、糖尿病(P=0.004)、既往心肌梗死病史(P=0.022)、既往心绞痛史(P<0.01)、抗血小板药物服用史(P=0.003)之间差异具有统计学意义。其中,ST段抬高组和无偏移组男性患者所占比例明显高于ST段压低组(P<0.05);ST段压低组糖尿病患者所占比例明显高于ST段抬高组和无偏移组(P<0.05)。三组患者LVEF差异无统计学意义。见表 1。
| 临床基线特征 | ST段抬高组(n=161) | ST段无偏移组(n=28) | ST段压低组(n=43) | χ2/F值 | P值 |
| 年龄(Mean±SD) | 56.2± 11.9 | 57.2± 12.6 | 59.2± 11.4 | 1.074 | 0.343 |
| 男性(n, %) | 138(85.7)a | 22(78.6)b | 21(48.8) | 26.915 | 0.001 |
| 吸烟(n, %) | 102(63.4) | 18(64.3) | 23(53.5) | 1.491 | 0.474 |
| 饮酒史(n, %) | 78(48.4) | 14(50.0) | 16(37.2) | 1.875 | 0.392 |
| 高血压病史(n, %) | 80(49.7) | 13(46.4) | 26(60.5) | 1.879 | 0.391 |
| 糖尿病病史(n, %) | 35(21.7)a | 4(14.3)b | 19(44.2) | 11.069 | 0.004 |
| 血脂异常(n, %) | 35(21.7) | 12(42.9) | 10(23.3) | 5.789 | 0.055 |
| 脑卒中史(n, %) | 18(11.2) | 1(3.6) | 7(16.3) | 2.601 | 0.265c |
| 冠心病家族史(n, %) | 29(18.0) | 6(21.4) | 6(14.0) | 0.693 | 0.707 |
| 既往心梗病史(n, %) | 13(8.1)a | 2(7.1) | 10(23.3) | 7.292 | 0.022c |
| 既往心绞痛史(n, %) | 46(28.6)a | 12(42.9) | 29(67.4) | 22.267 | 0.001 |
| PCI史(n, %) | 11(6.8) | 3(10.7) | 2(4.7) | 1.093 | 0.602c |
| 抗血小板药物服用史(n, %) | 24(14.9)a | 8(28.6) | 16(37.2) | 11.492 | 0.003 |
| 他汀类药物服用史(n, %) | 25(15.5) | 7(25.0) | 12(27.9) | 4.138 | 0.126 |
| LVEF(Mean±SD) | 51.0±6.7 | 51.0±6.4 | 49.5±6.3 | 0.981 | 0.377 |
| 注:抬高组和压低组比较,aP < 0.05;无偏移组和压低组比较, bp < 0.05; CFisher精确概率法 | |||||
3组患者之间梗死相关动脉(P < 0.01)、梗死部位(P=0.008)、闭塞病变(P < 0.01)、IRA侧枝循环形成(P < 0.01)以及病变血管支数(P=0.01)的差异具有统计学意义。ST段抬高组和压低组IRA以左冠状动脉前降支(left anterior descending coronary artery, LAD)和右冠状动脉(right coronary artery, RCA)多见,且梗死部位多位于近中段;而ST段无偏移组的IRA以左回旋支(left circumflex artery, LCX)多见,梗死部位多位于中远段。相比于ST段压低组,ST段抬高组和无偏移组患者的单支血管、闭塞病变所占比例较高(P<0.05)。相比于ST段抬高组,ST段无偏移组和压低组患者IRA形成侧枝循环的比例较高(P<0.05)。见表 2。
| 冠脉造影结果 | ST段抬高组(n=161) | ST段无偏移组(n=28) | ST段压低组(n=43) | χ2值 | P值 |
| 梗死相关动脉(n, %) | 38.141 | < 0.001 | |||
| LAD | 77(47.8) | 7(25.0) | 22(51.2) | ||
| LCX | 19(11.8)c | 17(60.7)b | 8(18.6) | ||
| RCA | 65(40.4)c | 4(14.3) | 13(30.2) | ||
| 梗死部位(n, %) | 13.893 | 0.008 | |||
| 近段 | 75(46.6)c | 4(14.3)b | 20(46.5) | ||
| 中段 | 53(32.9)c | 18(64.3)b | 12(27.9) | ||
| 远段 | 33(20.5) | 6(21.4) | 11(25.6) | ||
| 闭塞病变(n, %) | 110(68.3)a | 19(67.9)b | 13(30.2) | 21.330 | < 0.001 |
| IRA侧枝循环(n, %) | 26(16.1)a, c | 10(35.7) | 25(58.1) | 32.334 | < 0.001 |
| 病变支数(n, %) | 18.209 | < 0.001 | |||
| 1 | 58(36.0)a | 11(39.3)b | 2(4.7) | ||
| 2 | 55(34.2) | 8(28.6) | 18(41.9) | ||
| 3 | 48(29.8)a | 9(32.1) | 23(53.5) | ||
| 注:抬高组和压低组比较,aP < 0.05;无偏移组和压低组比较, bp < 0.05;抬高组和无偏移组比较,P < 0.05 | |||||
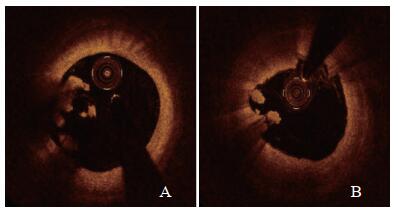
OCT下冠脉内红色血栓和白色血栓见图 2。ST段抬高组及无偏移组多表现为红色血栓,ST段压低组多表现为白色血栓。差异具有统计学意义(P<0.01)。3组OCT结果见表 3。
|
| A为红色血栓; B为柏色血栓 图 2 OCT下冠脉内血栓类型 Fig 2 Types of intracoronary thrombus guided by OCT |
|
|
| 指标 | ST段抬高组(n=161) | ST段无偏移组(n=28) | ST段压低组(n=43) | χ2值 | P值 |
| 血栓类型(例, %) | 26.678 | < 0.001 | |||
| 红色血栓 | 123(76.4)a | 18(64.3)b | 15(34.9) | ||
| 白色血栓 | 38(23.6)a | 10(35.7)b | 28(65.1) | ||
| 注:抬高组和压低组比较,aP < 0.05;无偏移组和压低组比较, bp < 0.05 | |||||
OCT因其较高的分辨率而在冠脉介入手术中得到广泛应用。除了能够辨别斑块类型、指导支架选择、判断内膜增生外[11-12],OCT还可用于冠脉内血栓类型的判断[13]。研究[14-15]表明,在OCT下红色血栓表现为一层强信号带后的信号衰减,而白色血栓表现为均匀信号、反射弱且无阴影。本研究中利用OCT判断冠脉内血栓类型,具有简单、准确的优点。
本研究中,ST段抬高组患者罪犯血管以LAD和RCA多见,且梗死部位多位于近中段;该组患者单支血管、闭塞病变所占比例较高;冠脉内血栓类型大多为红色血栓,与传统理论一致[1, 16]。ST段压低组患者女性患者所占比例高,糖尿病、既往心肌梗死、心绞痛、抗血小板药物服用史相对多见;其冠脉病变以多支血管病变为主,且多存在侧支循环;其冠脉内血栓类型以白色血栓为主。该类患者由于既往存在心肌梗死或心绞痛,在长期慢性缺血缺氧的条件下形成侧枝循环;因此当再次发生急性冠脉缺血事件时,冠脉血管由于存在缺血预适应,从而表现为非闭塞性病变[17];其多形成富含血小板的白色血栓可能与局部非中断的血流可冲走凝血酶有关。ST段无偏移组患者与ST段抬高组患者临床特征相近,表现在临床基线资料、冠脉造影中单支血管、闭塞病变所占比例以及冠脉内红色血栓所占比例。因此,推测ST段无偏移型心肌梗死与ST段抬高型心肌梗死有相似的病理生理学机制,即大多表现为不稳定粥样斑块的破裂,继发血栓形成导致管腔完全闭塞。其血栓类型主要与血栓形成机制相关:在血栓形成初期,血小板与内皮下vW因子结合后血小板被激活,发生黏附、聚集、释放反应,形成血小板小堆,之后激活内、外源性凝血系统,凝血酶原转变为凝血酶,激活纤维蛋白原转变为纤维蛋白,纤维蛋白网络红细胞、炎性细胞等继而形成红色血栓[18-19]。
本研究中,ST段无偏移组与ST段抬高者不同的是,其罪犯血管以LCX多见,且梗死部位多位于中远段;另外,ST段无偏移组患者IRA形成侧支循环的比例稍高。根据心脏解剖,回旋支中远段主要支配左室下壁、近心尖部心肌的血液供应。该处另有前降支和(或)右冠状动脉之后降支提供血供,因此,回旋支中远段闭塞后,该部位血供影响相对较小[20-21];加之标准十八导联心电图对血管远段病变的检测敏感性较低[22],因此心电图上可不表现为ST段抬高。有研究显示,当AMI的罪犯血管为LCX时,接近50%患者表现为急性非ST段抬高型心肌梗死[23]。另外,侧支循环的开放为梗死心肌提供了良好的血供,增加了心肌细胞对缺血缺氧的耐受性,某种程度上降低了心肌细胞的损伤程度,从而不表现为ST段的抬高。
对无明显ST段抬高的单支血管闭塞病变的AMI患者的研究,发现该类患者冠脉病变多以回旋支、较大的对角支或钝缘支闭塞为主,此类患者无明显ST段抬高与梗死部位为心电图相对不敏感的区域有关[24],同时,此类闭塞血管供血范围相对偏小,缺血心电向量相对较小[25]。推测这类患者与本研究中ST段无偏移组患者具有相似之处。
本研究根据心电图ST段改变对AMI的进一步分类具有一定创新意义。现有指南根据心电图ST段是否抬高,将AMI分为STEMI和NSTEMI [26-27]。然而,在临床上,对于ST段无偏移AMI患者,其临床症状、心电图改变不典型,容易延误诊治。本研究在课题组前期的工作基础上,将AMI分为ST段抬高组、ST段无偏移组和ST段压低组,发现ST段无偏移组与ST段抬高组具有相似的临床特征,多表现为单支血管、闭塞病变,形成红色血栓。因此,建议对ST段无偏移AMI患者采取积极的血运重建治疗。
利益冲突 所有作者均声明不存在利益冲突。
| [1] | Vogel B, Claessen BE, Arnold SV, et al. ST-segment elevation myocardial infarction[J]. Nat Rev Dis Primers, 2019, 5: 39. DOI:10.1038/s41572-019-0090-3 |
| [2] | Chen GX. Effects of intracoronary injection of nicorandil and tirofiban on myocardial perfusion and short-term prognosis in elderly patients with acute ST-segment elevation myocardial infarction after emergency PCI[J]. World J Emerg Med, 2020, 11(3): 157. DOI:10.5847/wjem.j.1920-8642.2020.03.005 |
| [3] | Malta Hansen C, Wang TY, Chen AY, et al. Contemporary patterns of early coronary angiography use in patients with non–ST-segment elevation myocardial infarction in the United States[J]. JACC: Cardiovasc Interv, 2018, 11(4): 369-380. DOI:10.1016/j.jcin.2017.12.016 |
| [4] | Grenne B, Eek C, Sjoli B, et al. Acute coronary occlusion in non-ST-elevation acute coronary syndrome: outcome and early identification by strain echocardiography[J]. Heart, 2010, 96(19): 1550-1556. DOI:10.1136/hrt.2009.188391 |
| [5] | Hung CS, Chen YH, Huang CC, et al. Prevalence and outcome of patients with non-ST segment elevation myocardial infarction with occluded "culprit" artery – a systemic review and meta-analysis[J]. Crit Care, 2018, 22: 34. DOI:10.1186/s13054-018-1944-x |
| [6] | Ino Y, Kubo T, Tanaka A, et al. Difference of culprit lesion morphologies between ST-segment elevation myocardial infarction and non–ST-segment elevation acute coronary syndrome[J]. JACC: Cardiovasc Interv, 2011, 4(1): 76-82. DOI:10.1016/j.jcin.2010.09.022 |
| [7] | 董淑娟, 楚英杰, 贺文奇, 等. 急性心肌梗死心电图ST段不同改变与冠脉造影病变特点的相关性[J]. 中华急诊医学杂志, 2013, 22(1): 29-30. DOI:10.3760/cma.j.issn.1671-0282.2013.01.018 |
| [8] | 张明, 楚英杰, 董淑娟, 等. 三种ST段不同表现的心肌梗死患者造影特征分析[J]. 医药论坛杂志, 2020, 41(06): 41-44. |
| [9] | Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018)[J]. Circulation, 2018, 138(20): 1-34. DOI:10.1161/cir.0000000000000617 |
| [10] | Wagner GS, Macfarlane P, Wellens H, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part Ⅵ: acute ischemia/infarction: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology[J]. J Am Coll Cardiol, 2009, 53(11): 1003-1011. DOI: 10.1016/j.jacc.2008.12.016. |
| [11] | Kim Y, Johnson TW, Akasaka T, et al. The role of optical coherence tomography in the setting of acute myocardial infarction[J]. J Cardiol, 2018, 72(3): 186-192. DOI:10.1016/j.jjcc.2018.03.004 |
| [12] | Jiang J, Tian NL, Cui HB, et al. Post-dilatation improves stent apposition in patients with ST-segment elevation myocardial infarction receiving primary percutaneous intervention: A multicenter, randomized controlled trial using optical coherence tomography[J]. World J Emerg Med, 2020, 11(2): 87-92. DOI:10.5847/wjem.j.1920-8642.2020.02.004 |
| [13] | Porto I, Mattesini A, Valente S, et al. Optical coherence tomography assessment and quantification of intracoronary Thrombus: Status and perspectives[J]. Cardiovasc Revascularization Med, 2015, 16(3): 172-178. DOI:10.1016/j.carrev.2015.01.007 |
| [14] | Kume T, Akasaka T, Kawamoto T, et al. Assessment of coronary arterial Thrombus by optical coherence tomography[J]. Am J Cardiol, 2006, 97(12): 1713-1717. DOI:10.1016/j.amjcard.2006.01.031 |
| [15] | Opolski M, Spiewak M, Marczak M, et al. TCT-632 mechanisms of myocardial infarction in patients with nonobstructive coronary artery disease: results from the optical coherence tomography study[J]. J Am Coll Cardiol, 2018, 72(13): B252-B253. DOI:10.1016/j.jacc.2018.08.1836 |
| [16] | 董淑娟, 龙东阳, 楚英杰, 等. "急诊PCI"模式下急性ST段抬高心肌梗死合并早期左心室血栓的危险因素分析[J]. 中华急诊医学杂志, 2020, 29(3): 386-391. DOI:10.3760/cma.j.issn.1671-0282.2020.03.016 |
| [17] | Hwang H, Park C, Cho J, et al. Clinical characteristics of occluded culprit arteries and collaterals in patients with non-ST-segment elevation myocardial infarction and impact on clinical outcomes[J]. Exp Ther Med, 2018, 16(4): 3710-3720. DOI:10.3892/etm.2018.6605 |
| [18] | Furie B, Furie BC. Mechanisms of Thrombus formation[J]. N Engl J Med, 2008, 359(9): 938-949. DOI:10.1056/nejmra0801082 |
| [19] | Raphael CE, Heit JA, Reeder GS, et al. Coronary embolus[J]. JACC: Cardiovasc Interv, 2018, 11(2): 172-180. DOI:10.1016/j.jcin.2017.08.057 |
| [20] | Stribling WK, Kontos MC, Abbate A, et al. Left circumflex occlusion in acute myocardial infarction (from the national cardiovascular data registry)[J]. Am J Cardiol, 2011, 108(7): 959-963. DOI:10.1016/j.amjcard.2011.05.027 |
| [21] | Chen PF, Tang L, Pei JY, et al. Prognostic value of admission electrocardiographic findings in non-ST-segment elevation myocardial infarction[J]. Clin Cardiol, 2020, 43(6): 574-580. DOI:10.1002/clc.23349 |
| [22] | Izumi C, Iga K, Kijima T, et al. Limitations of electrocardiography in the diagnosis of acute myocardial infarction. Comparison with two-dimensional echocardiography[J]. Intern Med, 1995, 34(11): 1061-1063. DOI:10.2169/internalmedicine.34.1061 |
| [23] | Moustafa A, Abi-Saleh B, El-Baba M, et al. Anatomic distribution of culprit lesions in patients with non-ST-segment elevation myocardial infarction and normal ECG[J]. Cardiovasc Diagn Ther, 2016, 6(1): 25-33. DOI:10.3978/j.issn.2223-3652.2015.10.05 |
| [24] | Khan AR, Golwala H, Tripathi A, et al. Impact of total occlusion of culprit artery in acute non-ST elevation myocardial infarction: a systematic review and meta-analysis[J]. Eur Heart J, 2017, 38(41): 3082-3089. DOI:10.1093/eurheartj/ehx418 |
| [25] | 魏宇淼, 陈芬, 邓珊, 等. 无明显ST段抬高的急性单支冠状动脉完全血栓闭塞所致急性心肌梗死临床特征分析[J]. 临床心血管病杂志, 2015, 6: 594-597. |
| [26] | Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC)[J]. Eur Heart J, 2018, 39(2): 119-177. DOI:10.1093/eurheartj/ehx393 |
| [27] | 中国医师协会急诊医师分会, 国家卫健委能力建设与继续教育中心急诊学专家委员会, 中国医疗保健国际交流促进会急诊急救分会. 急性冠脉综合征急诊快速诊治指南(2019)[J]. 中华急诊医学杂志, 2019, 28(4): 421-428. DOI:10.3760/cma.j.issn.1671-0282.2019.04.003 |
 2020, Vol. 29
2020, Vol. 29




