严重脓毒症及脓毒性休克时有效循环血量不足、血管床舒缩障碍和心肌收缩减退引起的循环功能衰竭、组织缺氧和多器官功能障碍综合征(MODS),是导致死亡最重要的原因[1-2]。脓毒症的预后与及时诊断及心血管功能评估与维护密切相关。目前临床上对脓毒性休克时心脏或心肌损害的评估除心脏超声和血流动力学监测外,参考心肌肌钙蛋白Ⅰ(cardiac troponin Ⅰ, cTnI)、肌酸激酶同工酶(creatine kinase isoenzymes, CK-MB)和N末端脑钠利肽(N-terminal fragment of B-type natriuretic peptide, NT-BNP)等生物学指标,但仍不能及时早期了解心肌损害情况,影响治疗措施的进行和预后判断。因此,探索心脏损害的标志物用于快速评估儿童严重脓毒症及脓毒性休克心肌受累及预后判断具有重要的意义。
脂肪酸结合蛋白是一种新型小胞质蛋白,在机体脂肪酸摄取、转运和代谢过程中起重要作用,其中心型脂肪酸结合蛋白(heart-type fatty acid-binding protein, H-FABP)具有高度心脏特异性,近年来发现其是评价心肌组织损伤的一种敏感的新型生物标志物。正常情况下血液中检测不到,但能从损伤的心肌组织中快速释放到血液中。有报道H-FABP可作为心肌梗死标志物,可在心肌细胞损伤后(1.5 h)快速释放至血液中,经肾脏代谢又可快速(24 h)恢复至正常水平,同时也是对急性冠状动脉综合征患者长期病死率预测的重要标志物[3-4]。
脓毒症的心肌损害与循环障碍是临床重要关注。约50%严重脓毒症及脓毒性休克发生心肌损害与心血管功能障碍[5-6],合并心肌损害时病死率明显升高[7-9]。少量报道成人严重脓毒症患者测定H-FABP可以预测患者预后,高H-FABP时预后不良[10-11]。儿童脓毒性休克与成人存在很大差异,特别容易引起心功能障碍、心肌损害和循环功能不稳定[12-13]。迄今,儿童严重脓毒症及脓毒性休克时H-FABP的变化与预后及心肌损害的关系无资料可循。为探索儿童严重脓毒症时H-FABP的变化,以及与传统心肌损害标志物的关系,2016年10月至2017年9月,笔者观察上海交通大学附属儿童医院重症医学科收治的儿童严重脓毒症与脓毒性休克H-FABP水平,并与cTnI、CK-MB、NT-BNP进行比较,现报道如下。
1 资料与方法 1.1 一般资料前瞻性观察2016年10月至2017年9月上海交通大学附属儿童医院重症医学科收治的严重脓毒症及脓毒性休克患儿78例,依据28 d生存情况分为死亡组(14例)与存活组(64例)。诊断标准参照2012年“Surviving sepsis campaign”严重脓毒症及脓毒性休克管理国际指南[14]及中国儿童脓毒性休克(感染性休克)诊治专家共识(2015版)[15]。严重脓毒症定义为宿主对感染的反应失控导致危及生命的器官功能衰竭,脓毒性休克定义为脓毒症患者尽管充分的液体复苏仍存在持续的低血压,需要使用升压药物维持正常血压,血乳酸(lactic acid,Lac)2 mmol/L以上。排除标准:先天性心脏病、冠状动脉疾病、心肌病、慢性心功能不全、心脏瓣膜病变、慢性肾功能不全、出血性休克、肌肉损伤的患者。研究方法经医院伦理委员会批准(批准文号:2016R007-P01)。
1.2 观察指标记录患儿年龄、性别、体质量指数等基线资料,于入院6 h内完善PRISM Ⅲ评分,留取EDTA抗凝血,留取血浆用于测定H-FABP和传统心肌损害标志物,包括cTnI、CK-MB、NT-BNP、LDH等。24 h内完成床旁心脏超声、床旁连续无创超声心输出量监测(ultrasound cardiac output monitoring,USCOM)等。记录左心室射血分数(left ventricular ejection fraction,LVEF)、左心室舒张末期内径(left ventricular end-diastolic dimension,LVEDD)、心脏指数(cardiac index,CI)、外周血管阻力(systemic vascular resistance index, SVRI)等。记录出院病死率及28 d病死率。心肌标志物均由本院检验科测定,H-FABP测定采用胶乳免疫比浊法测定法(Roche cobas c311全自动生化分析仪,试剂为北京九强生物技术股份有限公司生产);cTnI采用免疫层析法测定(RAMP锐普诊断仪,试剂为Response Biomedical Corporation公司生产);NT-BNP采用双向侧流免疫法(瑞莱RELIA-11分析仪,试剂为ReLIA瑞莱生物生产);LDH、CK-MB采用比色法(罗氏Cobas c 501全自动生化仪及试剂盒)。
1.3 统计学方法用SPSS 20.0统计学软件分析。符合正态分布的计量资料用均数±标准差(x±s),两组间比较采用成组t检验;不符合正态分布的计量资料采用中位数(25百分位,75百分位),两组间比较采用非参数秩和检验;计数资料采用例数或率表示,组间差异采用χ2检验;采用受试者工作特征(receiver operating characteristic, ROC)曲线及Kaplan-meier生存曲线分析评估血浆心肌损伤标记物与儿童严重脓毒症和脓毒症休克患者28 d病死率的关系。Kaplan-meier生存曲线组间对比分析采用Log-Rank检验。以P < 0.05为差异有统计学意义。
2 结果 2.1 基本情况比较同期符合观察标准的严重脓毒症及脓毒性休克患儿合计78例,其中男性46例(59.0%),女性32例(41.0%);年龄2~159个月龄,中位数16个月龄;严重脓毒症33例(42.3%),脓毒性休克45例(57.7%);死亡14例(17.9%),存活64例(82.1%)。对比死亡组和生存组的患者基线资料,PRISM Ⅲ评分、Lac水平和凝血酶时间(PT)在死亡组[分别为25.5(12,27.75),(6.63±4.89)mmol/L,(17.41±6.08)s]显著高于存活组[分别为11.2(10, 15),2.29±1.59 mmol/L,(13.36±1.64)s],两组间差异有统计学意义(P < 0.05),见表 1。两组原发感染部位比较,死亡组原发于呼吸道、胃肠道的感染高于存活组,两组间差异有统计学意义(P < 0.05),见表 1。
| 指标 | 死亡组(n=14) | 存活组(n=64) | χ2/t值 | P值 |
| 男/女(例) | 11/3 | 35/29 | 2.708 | 0.1 |
| 年龄(月) | 13.5(4-159) | 16(2-159) | -0.134 | 0.894 |
| BMI(kg/m2) | 17.50±3.64 | 16.90±2.55 | 0.56 | 0.579 |
| 收缩压(mmHg) | 86.88±16.1 | 98.86±16.0 | -1.919 | 0.062 |
| 舒张压(mmHg) | 50.25±18.9 | 56.78±11.8 | -1.269 | 0.211 |
| 心率(次/min) | 145±46 | 138±35 | 0.447 | 0.657 |
| PRISM Ⅲ | 25.5(12,27) | 11.2(10,15) | -4.281 | 0.000 |
| 乳酸(mmol/L) | 6.63±4.89 | 2.29±1.59 | 4.525 | 0.000 |
| 肌酐(μmoI/L) | 55.00±47.91 | 37.51±40.32 | 1.077 | 0.288 |
| 白细胞(109/L) | 17.61±10.67 | 14.30±9.68 | 0.861 | 0.394 |
| 血小板(109/L) | 108±153 | 179±151 | -1.199 | 0.237 |
| 凝血酶时间(PT)(s) | 17.41±6.08 | 13.36±1.64 | 3.615 | 0.001 |
| 纤维蛋白原(g/L) | 1.74±1.09 | 2.53±13.24 | -0.801 | 0.428 |
| 原发感染部位(例) | ||||
| 呼吸系统 | 10 | 19 | 8.569 | 0.003 |
| 肠道 | 2 | 31 | 5.489 | 0.019 |
| 泌尿系统 | / | 5 | 1.169 | 0.28 |
| 皮肤软组织 | / | 5 | 1.169 | 0.28 |
| 其他 | 2 | 4 | 1.045 | 0.307 |
提示H-FABP与传统心肌标志物及心指数均有明显正相关(P < 0.05),见表 2。
| 指标 | CI | CKMB | cTnI | LDH | BNP |
| Pearson相关系数 | 0.444 | 0.914 | 0.345 | 0.537 | 0.622 |
| P值 | 0.002 | < 0.01 | 0.02 | < 0.01 | < 0.01 |
分析H-FABP、CK-MB、cTnI、LDH和NT-BNP,以及心超、USCOM监测指标在严重脓毒症及脓毒性休克患儿中的死亡组和存活组的差异,H-FABP、CK-MB、LDH、NT-BNP在死亡组[分别为49.10±65.14 ng/mL,131.63±130.91 U/L,2 403.88±415.97 U/L,2 498.5(615.58,13 075.75)pg/mL)均明显高于存活组[分别为(5.06±4.29)ng/mL, (37.30±29.24)U/L,(2 971.57±279.49)U/L,672(279.5,1753.5)pg/mL),两组间差异有统计学意义(P < 0.05或P < 0.01)。cTnI、CI、SVRI、LVEF和LVEDD在死亡组和生存组两组间差异无统计学意义(P > 0.05);见表 3。
| 指标 | 死亡组 | 存活组 | Z值 | P值 |
| H-FABP(ng/mL) | 49.10±65.14 | 5.06±4.29 | -3.148 | 0.002 |
| CK-MB(U/L) | 131.63±130.91 | 37.30±29.24 | -3.0 | 0.003 |
| cTnI(μg/L) | 0.50±0.88 | 0.11±0.17 | -1.755 | 0.079 |
| LDH(U/L) | 2 403.88±415.97 | 2 971.57±279.49 | -2.791 | 0.005 |
| NTBNP (pg/ml) |
2498.5 (615.58, 13 075.75) |
672 (279.5, 1 753.5) |
-2.004 | 0.045 |
| CI[L/(min·m2)] | 5.53±1.10 | 4.76±0.80 | -1.874 | 0.061 |
| SVRI [dyn.s/(cm5·m2)] |
946.25±303.87 | 1 192.00±263.37 | -1.885 | 0.058 |
| LVEF(%) | 65.00±2.83 | 66.92±3.83 | -1.431 | 0.152 |
| LVEDD | 2.53±0.18 | 2.91±0.64 | -1.756 | 0.079 |
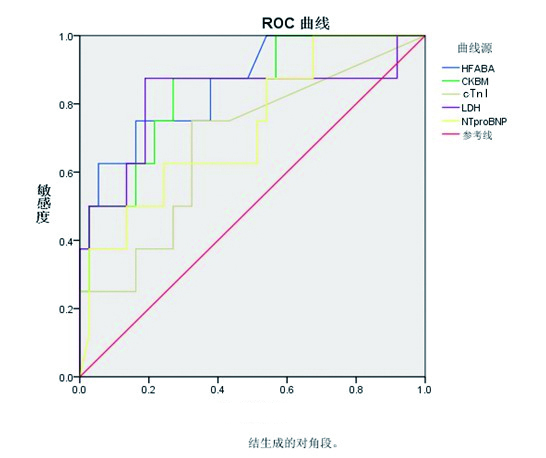
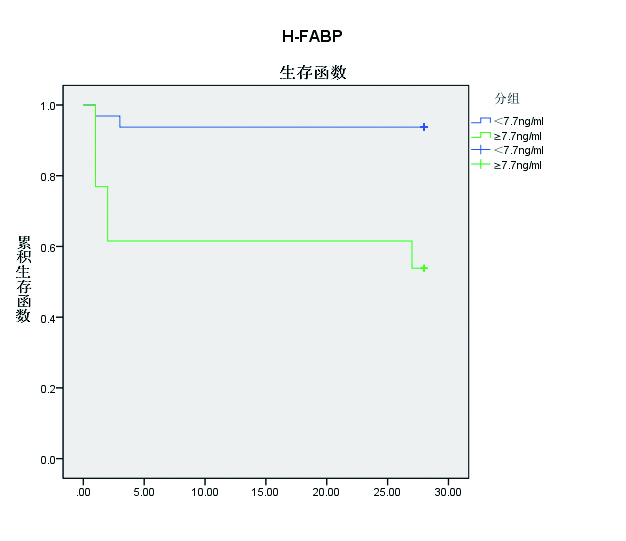
ROC曲线分析入PICU 6 h内H-FABP、CK-MB、cTnI、LDH、NTBNP预测28日生存状况(图 1)。H-FABP作为预测预后标记物的ROC曲线下面积(AUC)为0.858,95%置信区间(CI):0.716-1.0(P=0.002),优于CK-MB(AUC=0.841, 95%CI:0.696~0.986; P=0.003),LDH(AUC=0.818, 95%CI:0.610~1.000; P=0.005)和NT-BNP(AUC=0.728, 95%CI:0.535~0.921; P=0.045)。H-FABP预测儿童严重脓毒症和脓毒症休克患者28 d生存情况的截断值为7.7 ng/mL,对应的敏感度为75%,特异度为83.8%(见表 4和图 2)。进一步以H-FABP的ROC分析获取的截断值(7.7 ng/mL)分组,分为H-FABP≥7.7 ng/mL组和H-FABP < 7.7 ng/mL组;经Log-Rank对比分析Kaplan-Meier生存曲线,结果提示:H-FABP≥7.7 ng/mL组的28 d病死率显著高于H-FABP < 7.7 ng/mL组(P < 0.05)。
|
| 图 1 ROC曲线分析入PICU 6 h血浆H-FABP、CK-MB、cTnI、LDH、NTBNP预测严重脓毒症及脓毒性休克患儿28 d病死率情况 Figure 1 H-FABP, CK-MB, cTnI, LDH, NTBNP predicted 28-day mortality in children with severe sepsis and septic shock with Receiving operating characteristic curves |
|
|
| 指标 | 最大面积 | 截值 | 灵敏度 | 特异度 | P值 | 95%可信区间 | |
| 下限 | 上限 | ||||||
| H-FABP | 0.858 | 7.7 | 0.750 | 0.838 | 0.002 | 0.716 | 1.000 |
| CK-MB | 0.841 | 40.5 | 0.875 | 0.730 | 0.003 | 0.696 | 0.986 |
| cTnI | 0.686 | 0.04 | 0.750 | 0.676 | 0.103 | 0.476 | 0.895 |
| LDH | 0.818 | 557.5 | 0.875 | 0.811 | 0.005 | 0.610 | 1.000 |
| NTBNP | 0.728 | 1 653 | 0.625 | 0.757 | 0.045 | 0.535 | 0.921 |
|
| 图 2 入PICU 6 h内H-FABP≥7.7 ng/mL患儿组和H-FABP < 7.7 ng/mL患儿组的Kaplan-Meier生存曲线分析 Figure 2 Kaplan-Meier curves of H-FABP. The survival rate of patients for H-FABP < 7.7 ng/mL was higher than that of patients who H-FABP≥7.7 ng/mL were negative (P < 0.05) |
|
|
本文探讨H-FABP评估儿童严重脓毒症和脓毒症休克患者心肌损伤及与患者预后的关系。结果对78例患儿测定入PICU 6 h内血浆心肌损伤标记物并分析与患儿预后的关系,发现H-FABP是28 d病死率的有效预测指标,预测心肌损害优于cTnI、CK-MB、LDH和NT-BNP等传统心肌损害标志物。此结果与国内外成人脓毒症患者预后研究接近[10, 16-17],说明无论是成人还是儿童,H-FABP是预测严重脓毒症和脓毒症休克预后与心肌损害敏感标记物。
心血管功能障碍是脓毒症患儿的常见并发症,增加患者预后不良的风险。在小鼠试验中可发现脓毒症导致心肌损伤与TNF-α、IL-6和IL-8促炎因子有关,可见心肌细胞水肿,广泛心肌局部出血、坏死和大量的炎症细胞浸润[18]。Takasu等[19]对44例脓毒症患者心脏尸解发现:脓毒症常导致不同程度的心肌间质细胞纤维化、心肌细胞肥大和心肌细胞内线粒体肿胀。研究报道脓毒症前3 d心功能障碍发生率高达40%~60%,并导致脓毒症患者死亡风险增加[7-9]。成人脓毒症伴发心肌损伤病死率由20%上升至70%~90%[20],而儿童脓毒症更易出现心血管功能障碍,有报道发生率高达80%[12-13]。
传统超声心动图能有效评估左心室功能,但不能早期发现脓毒症相关心肌损伤及心功能障碍[1]。探索敏感性及特异性高的早期预警脓毒症心肌损害的心肌损伤标记物对早期及时维护心功能、降低脓毒症患者病死率具有重要意义。目前,已有研究报道心肌损伤分子标记物TnT和NT-BNP与脓毒症预后密切有关[21-23]。近年来,H-FABP作为心脏特异表达的新型小胞质蛋白在心肌受损早期0~3 h即可升高,已被当作心血管疾病的早期生物标志物和不良心脏事件的有效预后指标[9, 24]。Jeong等[25]研究了在急性冠脉综合征(acute coronary syndrome,ACS)、非ACS和传染性疾病患者的危险分层情况下,H-FABP是预测病死率的较好指标。并有研究发现H-FABP能早期鉴别心肌梗死、心源性晕厥、早期预测先天性心脏病的心功能不全[3, 4, 24, 26-27]。有报道H-FABP在ICU患者中比普通患者高,且可以预测ICU患者的90 d病死率[28]。然而,在儿童脓毒症患者中,血浆H-FABP水平和脓毒症患儿预后之间的关系尚未有系统资料可循。本组发现严重脓毒症及脓毒性休克患儿死亡组入PICU 6 h的血浆H-FABP、CK-MB、LDH、NT-BNP均较存活组显著升高(P < 0.05),但入PICU 24 h内心超和USCOM指标差异无统计学意义;这提示入PICU 6 h的血浆H-FABP、CK-MB、LDH、NT-BNP指标能较早的预警心肌损害,并且与死亡风险相关。进一步评估H-FABP、CK-MB、cTnI、LDH、NT-BNP预测患者28 d病死率的ROC曲线发现H-FABP优于传统的心肌酶谱,其AUC是0.858 (95%CI:0.716~1.0, P=0.002),截断值为7.7 ng/mL,对应敏感度和特异度分别达到75%和83.8%;且严重脓毒症及脓毒性休克患儿28 d生存率,H-FABP≥7.7 ng/mL时存活率显著下降(P < 0.05)。与Chen等[17]的研究报道相似,认为H-FABP在大于7 ng/mL时,成人脓毒症患者病死率增加。因此,H-FABP预测严重脓毒症及脓毒性休克患儿预后优于传统心肌酶谱,是脓毒症患儿28 d病死率的有效预测标记物。
本文尚有不足之处。首先,未对心肌损伤标记物动态监测。其次,部分数据受容量复苏和血管活性药物的影响,本研究难以厘清相互之间的关系。但本研究基于前瞻性病例收集和数据分析,明确了H-FABP是脓毒症患儿28 d病死率的有效预测标记物,且优于传统心肌酶谱。为进一步进行多中心、大范围临床研究进一步明确H-FABP与病情的关系提供了依据。
| [1] | Sevilla Berrios RA, O'Horo JC, Velagapudi V, et al. Correlation of left ventricular systolic dysfunction determined by low ejection fraction and 30-day mortality in patients with severe sepsis and septic shock: a systematic review and meta-analysis[J]. J Crit Care, 2014, 29(4): 495-499. DOI:10.1016/j.jcrc.2014.03.007 |
| [2] | Sanfilippo F, Corredor C, Fletcher N, et al. Diastolic dysfunction and mortality in septic patients: a systematic review and meta-analysis[J]. Intensive Care Med, 2015, 41(6): 1004-1013. DOI:10.1007/s00134-015-3748-7 |
| [3] | Kurz K, Giannitsis E, Becker M, et al. Comparison of the new high sensitive cardiac troponin T with myoglobin, h-FABP and cTnT for early identification of myocardial necrosis in the acute coronary syndrome[J]. Clin Res Cardiol, 2011, 100(3): 209-215. DOI:10.1007/s00392-010-0230-y |
| [4] | Banu S, Tanveer S, Manjunath CN. Comparative study of high sensitivity troponin T and heart-type fatty acid-binding protein in STEMI patients[J]. Saudi J Biol Sci, 2015, 22(1): 56-61. DOI:10.1016/j.sjbs.2014.05.011 |
| [5] | Y K, T I, M N, et al. Sepsis-induced myocardial dysfunction: pathophysiology and management[J]. J Intensive Care, 2016, 4(22). DOI:10.1186/s40560-016-0148-1 |
| [6] | L DG, J E, A O. Strain echocardiography in septic shock-a comparison with systolic and diastolic function parameters, cardiac biomarkers and outcome[J]. Crit Care, 2015, 19(1): 122. DOI:10.1186/s13054-015-0857-1 |
| [7] | Martin L, Derwall M, Thiemermann C, et al. Heart in sepsis: Molecular mechanisms, diagnosis and therapy of septic cardiomyopathy[J]. Anaesthesist, 2017, 66(7): 479-490. DOI:10.1007/s00101-017-0329-x |
| [8] | A A, A VB. Cardiac dysfunction in sepsis[J]. Intensive Care Med, 2016, 42: 2073-2076. DOI:10.1007/s00134-016-4503-4 |
| [9] | Jayaprakash N, Gajic O, Frank RD, et al. Elevated modified shock index in early sepsis is associated with myocardial dysfunction and mortality[J]. J Crit Care, 2018, 2(43): 30-35. DOI:10.1016/j.jcrc.2017.08.019 |
| [10] | Jo YH, Kim K, Lee JH, et al. Heart-type fatty acid-binding protein as a prognostic factor in patients with severe sepsis and septic shock[J]. Am J Emerg Med, 2012, 30(9): 1749-1755. DOI:10.1016/j.ajem.2012.02.005 |
| [11] | Zhang ZC, Dai HW, Yu YH, et al. Usefulness of heart-type fatty acid-binding protein in patients with severe sepsis[J]. J Crit Care, 2012, 27(4): 415. e13-8. DOI:10.1016/j.jcrc.2012.01.004 |
| [12] | Price S, Anning PB, Mitchell JA, et al. Myocardial drsfunction in sepsis: mechanisms and therapeutic implications[J]. Eur Heart J, 1999, 29(10): 715-724. |
| [13] | Feltes TF, Pignatelli R, Kleinert S, et al. Quantitated left ventricular systolic mechanics in children with septic shock utilizing noninvasive wall stress analysis[J]. Crit Care Med, 1994, 22: 1647-1658. DOI:10.1097/00003246-199422100-00022 |
| [14] | Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guideline for management of severe sepsis andseptic shock: 2012[J]. Crit Care Med, 2013, 41(2): 580-637. DOI:10.1097/CCM.0b013e31827e83af |
| [15] | 中华医学会儿科学分会急救学组. 儿童脓毒性休克(感染性休克)诊治专家共识(2015版)[J]. 中华儿科杂志, 2015, 53(8): 576-580. |
| [16] | 李丹丹, 李雯莉, 高冉冉, 等. 心肌脂肪酸结合蛋白在脓毒症临床预后的预测价值研究[J]. 中华急诊医学杂志, 2016, 25(11): 1443-1448. DOI:10.3760/cma.j.issn.1671-0282.2016.11.018 |
| [17] | Chen YX, Li CS. The prognostic and risk-stratified value of heart-type fatty acid-binding protein in septic patients in the emergency department[J]. J Cri Care, 2014, 29(4): 512-516. DOI:10.1016/j.jcrc.2014.03.026 |
| [18] | Qin YJ, Zhang XL, Yu YQ, et al. Cardioprotective effect of erythropoietin on sepsisinduced myocardial injury in rats[J]. World J Emerg Med, 2013, 4(3): 215-222. DOI:10.5847/wjem.j.1920-8642.2013.03.011 |
| [19] | Takasu O, Gaut JP, Watanabe E, et al. Mechanisms of cardiac and renal dysfunction in patients dying of sepsis[J]. Am J Respir Crit Care Med, 2013, 187(5): 509-517. DOI:10.1164/rccm.201211-1983OC |
| [20] | Parrillo JE, Parker MM, Natanson C, et al. Septic shock in humans: advances in the understanding of pathogenesis, cardiovascular dysfunction, and therapy[J]. Ann Intern Med, 1990, 113(3): 227-242. DOI:10.7326/0003-4819-113-3-227 |
| [21] | 黄娇甜, 祝益民, 卢秀兰. 重症监护室脓毒症患儿心肌损伤的临床研究[J]. 中华实用儿科临床杂志, 2011, 26(6): 423-426. DOI:10.3969/j.issn.1003-515X.2011.06.013 |
| [22] | Vallabhajosyula S, Sakhuja A, Geske JB, et al. Role of admission troponin-t and serial troponin-T testing in predicting outcomes in severe sepsis and septic shock[J]. J Am Heart Assoc, 2017, 6(9): P Ⅱ : e005930. DOI:10.1161/JAHA.117.005930 |
| [23] | Masson S, Caironi P, Fanizza C, et al. Sequential N-terminal pro-B-type natriuretic peptide and high-sensitivity cardiac troponin measurements during albumin replacement in patients with severe sepsis or septic shock[J]. Crit Care Med, 2016, 44(4): 707-716. DOI:10.1097/CCM.0000000000001473 |
| [24] | Zhou FJ, Zhou CY, Tian YJ, et al. Diagnostic value of analysis of H-FABP, NT-proBNP, and cTnI in heart function in children withcongenital heart disease and pneumonia[J]. Eur Rev Med Phamacol Sci, 2014, 18(10): 1513-1516. |
| [25] | Jeong JH, Seo YH, Ahn JY, et al. The prognostic value of serum levels of heart-type fatty acid binding protein and high sensitivity C-reactive protein in patients with increased levels of amino-terminal pro-B type natriuretic peptide[J]. Ann Lab Med, 2016, 36(5): 420-426. DOI:10.3343/alm.2016.36.5.420 |
| [26] | Sönmez B. M., Öztürk D., Yilmaz F, et al. Bedside heart type fatty acid binding protein (H-FABP): Is an early predictive marker of cardiac syncope[J]. J Pak Med Assoc, 2015, 65(1): 1156-1160. |
| [27] | Hamza M, Demerdash S, Ibrahim M. Heart-type fatty acid-binding protein as a diagnostic biochemical marker for early detection of myocardial infarction[J]. Acta Cardiol, 2016, 71(5): 537-541. DOI:10.2143/AC.71.5.3167496 |
| [28] | Shirakabe A, Kobayashi N, Hata N, et al. Prognostic impact of the serum heart-type fatty acid-binding protein (H-FABP) levels in patients admitted to the non-surgical intensive care unit[J]. Clin Res Cardiol, 2014, 103(10): 791-804. DOI:10.1007/s00392-014-0717-z |
 2018, Vol. 27
2018, Vol. 27




